Emergency Visit Roadmap
Why does it always feel like there’s so much waiting?
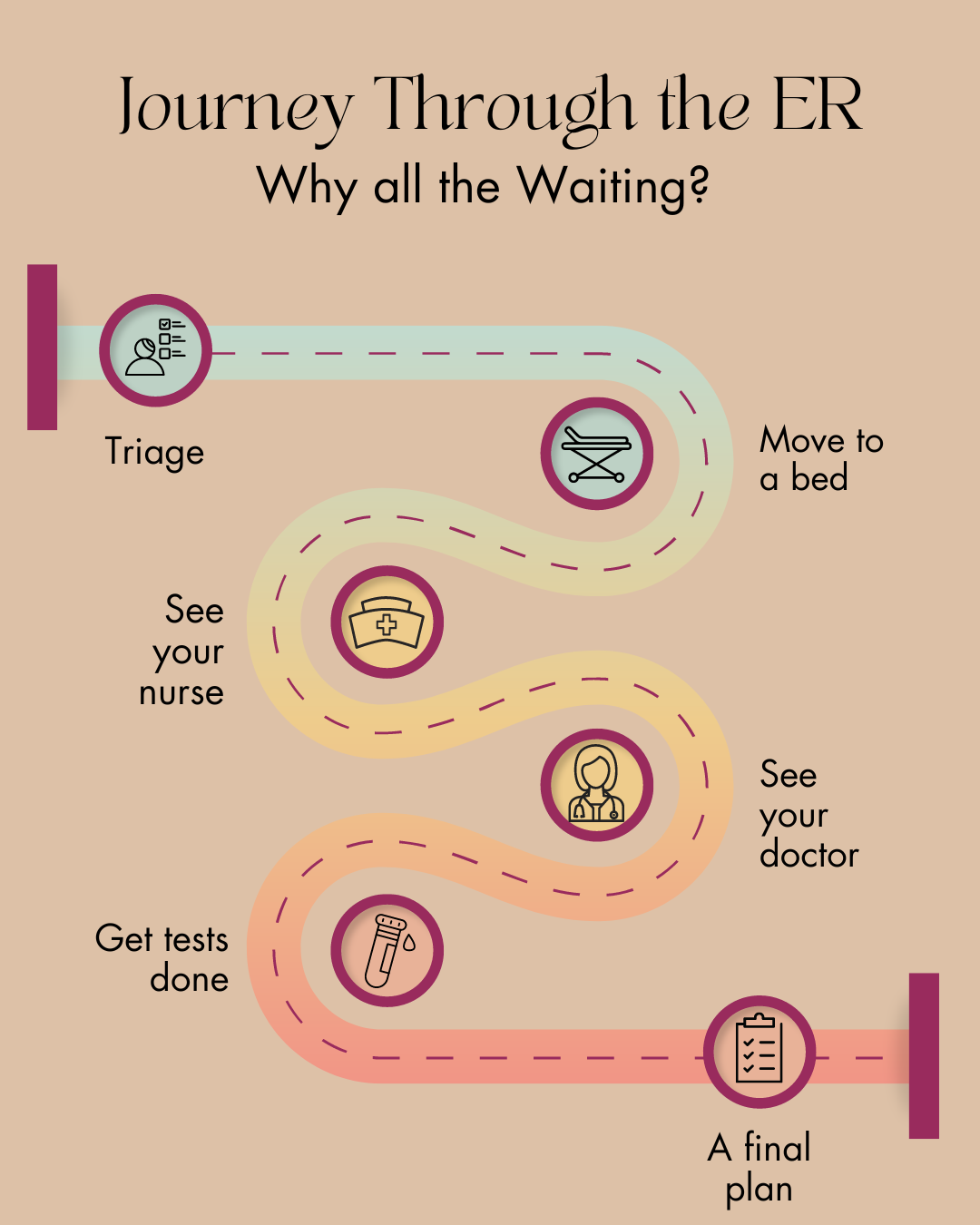
If you’ve ever been to the emergency room either yourself or with a friend of family member, there are many points along the ER journey that can feel like a lot of sitting around an waiting. As an ER doctor, I’d like to guide you through this journey to help you better understand why these waits are often necessary.
When You First Arrive
Whether by ambulance or walking in, the first step in your ER journey is always to get triaged. This occurs almost as soon as you enter the door. Depending how busy things are, there may be a line up to be triaged for those who are able to wait. The example of pediatric ERs during respiratory virus season comes immediately to mind as one of these times.
Once you do reach the triage desk, you’ll be assessed by a specialized triage nurse who will take your vital signs and a brief history. This information helps to decide what your “triage score” is (how urgently you need to be seen). If someone has a life or limb threatening injury, they are the most emergent category and get brought in right away. After you are triaged, you’re asked to wait in the waiting room until it’s your turn. This is often the longest wait in your ER journey, depending on how sick you are. If at any point, you’re worried your condition has worsened, please don’t be afraid to go back up to the triage desk to let them know - this is valuable information for the triage team.
Moving into the Emergency Department
When it’s your turn, you are brought into the main emergency department. Depending on the reason you are there, you may be brought directly to a stretcher, a recliner, or an internal waiting room chair. The first person you see will be the nurse assigned to you. There may be a wait between arriving in your space and seeing your nurse, depending how busy things are. Your nurse will take your vital signs, examine you, and take a brief history of why you are there. They may take some bloodwork at this time as well.
Next, you will see your doctor (or a learner working with your doctor). There is often a wait between when you are seen by your nurse and when you are seen by your doctor. Your doctor is often managing 10-20 other people at the same time - assessing them, ordering tests, reassessing them, making phone calls, and being pulled into rooms when very sick patients come in.
When your doctor comes in, they will do a history and physical exam to gather the necessary information to decide what tests, if any, need to be done. These tests will be ordered once your doctor leaves, and could include things like bloodwork or imaging tests. If you were first seen by a medical learner (student or resident), they will review your case with the doctor, who will then come back to see you as well.
Depending on why you are there, there are additional allied health providers that you may see, like social work, respiratory therapy, physiotherapy, pharmacy, or a transition coordinator, to name a few.
Waiting for Answers
Your nurse or phlebotomist will come and draw your bloodwork and sent it to the lab. If you’ve had imaging tests ordered, like x-ray, ultrasound, or CT scan, you’ll wait for your turn to get these done as well. Your doctor may have ordered some medications to be administered to help manage symptoms or treat a known condition, so these will be administer by your nurse as well.
There is often a long wait at this point, while your bloodwork and imaging results are coming back. The bloodwork alone can take an hour or more to be resulted, and the imaging tests are first looked at by your ER doctor, but often have to be reported by the on call radiologist as well. These things take time. Your doctor then has to interpret all of these results together to decide what the next steps are. Remember, your doctor is doing this for 10-20 other patients as well.
During this time, you’ll be reassessed by your nurse, who will relay this information to your doctor (who may come in to reassess you as well).
Putting it All Together
Once your doctor has received the results of all of your tests, they interpret them all in the context of your history and exam and decide what the next steps are. This could be any of the following scenarios:
going home with no follow up needed - for example a cold, a nosebleed that stops, a stomach bug
going home with follow up by either your family doctor or a specialist - for example a fracture that needs to be seen by orthopedics as an outpatient, high blood sugar with otherwise normal tests, stitches that need removal
going home with outpatient tests ordered - for example a stress test or holter monitor, an MRI, a return to the ER the next day for imaging
being admitted to hospital - for example appendicitis, pneumonia needing oxygen therapy, a heart attack or stroke
What if I Need to be Admitted?
If you need admission to hospital, your doctor will call the specific specialist on call, and someone from their team will then come to assess you. This will take time, depending on how many other consults that admitting team needs to see and how many issues they are dealing with for their already admitted patients in the hospital.
Once the admitting team has assessed you, they’ll put in your admission orders. A bed request is then made, so that when a bed is available on the wards, you’ll be moved to it. Unsurprisingly, this is very often associated with a wait as well.
What if I Need Outpatient Followup?
If you’ve been asked to see your family doctor, it’s important to make sure to call them as soon as you can to make that follow up appointment.
If you’ve been referred to a specialist or for more tests, most of the time their office will call you, but sometimes you may be given a number to call and make an appointment. Be sure to clarify this with your doctor before you are discharged.
I hope this gives you a better sense of why there is often a lot of waiting throughout the ER journey. Please be patient with us. I promise you we are doing the best we can for you.